Cancer changes relationships. I was once told a story about a lady diagnosed with breast cancer about 30-40 years ago. She was probably about my age and given 6 months to live. It turned out she lived longer than that (and is still alive in fact), but for the longest time she was never really given the “all clear”, like okay now we know you’re going to live for decades longer, not months. So 9 months would pass…then doctors would say, “Well you keep hanging in there, but you still only probably have a few months”. The story goes that at some point fairly early on she “picked” a future spouse for her husband, a family friend or something along those lines. Time goes on, she doesn’t die, and her husband ends up having an affair with the replacement. The lady and her husband get divorced, he ends up marrying the replacement, and the kids get very resentful and stop talking the husband. This story, like so many I’ve heard about the lives of cancer patients and fallout of a cancer diagnosis, does not surprise me at all. Once you get diagnosed with cancer a cloud of never-ending uncertainty will hang over you and those around you.
This year my husband and I are celebrating our 14th year of marriage. The longer I am married, the more I realize 1) marriage is hard (duh!) and 2) marriage is kind of a crap shoot. People change, in pretty major ways and in ways that put stress on the marriage, whether it be mild or extreme. I also observe that inevitably you and your spouse are going to split ways on one or more of the values and expectations that you thought you had all squared away before marriage. Kids change things in very complex ways. On one hand, kids bring a common goal to the relationship. You both want what’s best for them and, like a complicated, huge, life puzzle, you want to work together to navigate the best way to parent your children. You really want to put them on the best life path you can and do everything in your power to make them feel loved and resilient. Kids bring shared joys and memories. They bring this new love and excitement that can be really bonding for parents. On the other hand, no two people are ever going to parent the same way or agree on every parenting decision. And because kids are so important and valuable to parents, even the slightest difference of opinion can become a major source of tension. What I did not realize going into our marriage is that my husband would have so much confidence in child rearing (right out of the gate…like he thought he was an expert from day one….and in many ways it seemed like he was) and I would feel so incompetent. Breast feeding only intensified this phenomenon. As many women who breast feed will probably tell you, breast feeding an infant is one of the most difficult and rewarding things you might do as a mother and is extremely difficult and frustrating at the onset. Things generally do not go well from the get go with the first baby. In my case, my poor little baby was born on the small side and so any weight loss (which is normal after birth) was regarded as an emergency (not really, but in our eyes it was). My first born and I were having a terrible time getting him to consume any breast milk the first few days and he was not only miserable but also dropped to less than 6 lbs. We weren’t getting any sleep and finally in the middle of our 1st night home my husband, the baby expert, took our newborn and majestically gave him formula and single handedly “saved his life”. This made me feel like the biggest flop of a mother out there. I remember the next morning, at one of my most beaten down, downtrodden moments of motherhood, my husband, the baby expert, renaissance man that he is valiantly displayed the bottle to me and claimed “HE LOVED IT!”. Point being, I would say for my husband and I, the first year of parenthood was the most difficult of our marriage (he does not agree with this at all, but again, I think he was high on “daddy” hormones and his natural, God-given talent of being a dad). Through the years, as I’ve found my way in motherhood and gained more confidence, we have different battles, but I feel we’re on a more level playing field.
When preparing for marriage, we attended a very short workshop at a church, just to cover all the “premarital counselling” bases. One thing I remember is one of the teachers was telling us a story of how her husband was making a list of all of her faults one day. I was aghast, that sounded terrible to me. I felt like I already kept a pretty hefty tabulation of all my faults ready at moments notice to interfere with my goals and crush my dreams. I definitely didn’t need to add this dynamic to my life. And really, I found it hard to believe either my fiancé or I would ever stoop to the level of calling out your spouse’s faults. Well, 14 years into marriage, I can tell you some days all we do is revel in each other’s shortcomings. But for better or worse, we are a team, and I know we will always be committed to our partnership in this family.
I felt I should give my husband a fair shot in this marriage opinion piece, so I asked him. “If you were writing an article about your experiences with marriage, what you be your main points?” To which he answered, “I guess I’d say you forget what you fell in love with.” Dead silence. I get what he was trying to say, but what? So, I guess you have that. Maybe he can wordsmith that into a loving essay someday. As for me, without a doubt, within a snap of a finger, I know exactly what I fell in love with. His humor, it’s the best. So, there you go, Travis. I remember exactly. I appreciate his humor so much, that when I think of his flaws (which I do daily, it’s part of my job as a wife)…I always come back to his quick wit and ability to entertain and lighten the mood of whatever crowd he is in. As much as Travis likes to portray a dark and brooding mysterious character, he is very much the extrovert to my introvert. While I want to duck into a corner in the fetal position and cover my neck tornado-drill style when I enter a room full of people, Travis lights up like a Christmas tree. This combination doesn’t always work with other people. For me, and probably most other introverts, extroverts can drown me out and seemingly take away my voice in a relationship. In Travis, I have found my unicorn. Somehow he is able to use his sparkle to light up a room and help me feel comfortable in groups and yet still maintains the patience and understanding to listen to me and make me feel heard.
As I’ve observed other marriages and reflect on how my cancer diagnosis has affected our marriage, I would say overall the cancer has brought us into a closer partnership. That is not to say that cancer doesn’t bring its own challenges to a marriage. I’ve gone through some dramatic physical changes that I’m sure my husband did not see coming when we got married. I’ve lost hair, gained and lost weight depending on treatments, and lost both of my breasts. The constant appointments, health care decisions, and ever changing discomfort and treatment side effects that I experience all take their toll on both of us. While I don’t think hospitals and cancer are enjoyable for any spouse, Travis seems to have a particularly strong discomfort with medical problems and the healthcare system and to ask him to be my primary partner in all of this is hard. And on top of that, I just don’t have the energy and stamina that I did pre-cancer. So not only do we have all of the stress of a terminal illness diagnosis, but he also has to pick up the slack of normal life when I’m not up to it. And he does all of this without complaint.
As morbid as it sounds, sometimes in the back of my mind I feel like I’m prepping him for being a single parent. Does he know how the boys’ schedules work and how they might change? Is he ready to make arrangements if I do end up in the hospital or worse sooner than we expect? Does he understand and respect my parenting well enough to continue my influence if I’m not around? Is he resilient enough to carry on and be the steadfast leader of the family he may need to be much sooner than he expected when we said our vows 14 years ago? We are living the “in sickness” vows every day and it really challenges us at times. That being said, there are definitely “mid-life crisis”-like issues that I assume would be more at the forefront of our marriage if we didn’t have this cloud of my mortality hanging over us and distracting us. I am thankful that we have taken more time to enjoy each other, travel together, and grant each other grace because we know our time together may be limited. I’m not sure why it takes a cancer diagnosis to stop and smell the roses, but sometimes it does, and for that I am grateful.


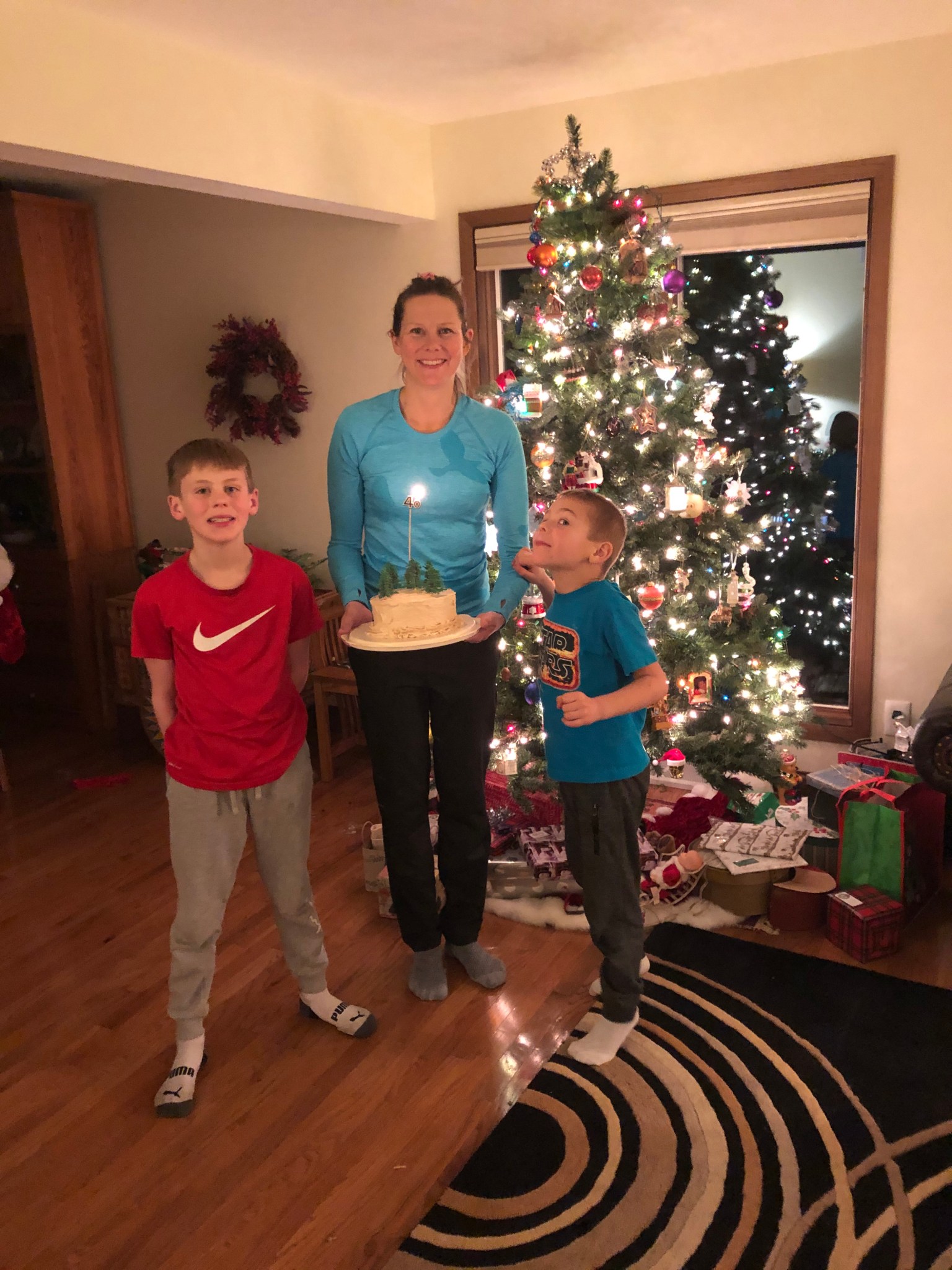 December was a big month for me. I turned 40 and celebrated my 2nd birthday and 2nd Christmas with metastatic breast cancer. Turning 40 was big for me, not because I expected to feel different, but because I have had two drastically different emotions pulling at me, gratitude and disappointment. I was diagnosed with what can be an extremely quick-moving terminal illness when I was 38. I am obviously thankful I have reached my forties and it doesn’t escape me that my luck continues to grow as the years go by. On the other hand, I had big plans for 40 that didn’t involve metastatic breast cancer. My plans specifically involved a big 5-year survival bash that would coincide with turning 40. Had my cancer not returned, this upcoming March would have marked my 5-year survival mark. This is the point at which the chance of a cancer recurrence becomes minimal, a real holy grail for any cancer survivor.
December was a big month for me. I turned 40 and celebrated my 2nd birthday and 2nd Christmas with metastatic breast cancer. Turning 40 was big for me, not because I expected to feel different, but because I have had two drastically different emotions pulling at me, gratitude and disappointment. I was diagnosed with what can be an extremely quick-moving terminal illness when I was 38. I am obviously thankful I have reached my forties and it doesn’t escape me that my luck continues to grow as the years go by. On the other hand, I had big plans for 40 that didn’t involve metastatic breast cancer. My plans specifically involved a big 5-year survival bash that would coincide with turning 40. Had my cancer not returned, this upcoming March would have marked my 5-year survival mark. This is the point at which the chance of a cancer recurrence becomes minimal, a real holy grail for any cancer survivor.